In hospitals and laboratories, sterilization is not treated as a formality. It is a responsibility. One improperly sterilized instrument can lead to infection, inaccurate test results, or serious safety risks. That is why the autoclave is considered essential equipment, not an optional one.
From operating theatres to microbiology labs, the autoclave machine is used daily to ensure materials are free from harmful microorganisms. It works quietly in the background, but its role is critical.
This guide explains autoclaves in a practical, real‑world manner — how they work, why they are trusted, and where they are used.
Table of Contents
ToggleWhat Is an Autoclave?
An autoclave is a sterilization device that uses pressurized steam to destroy bacteria, viruses, fungi, and spores. The combination of heat, moisture, and pressure makes this method extremely effective.
Surface disinfectants only reduce contamination. Autoclaving, when performed correctly, eliminates it completely. That is why autoclaves are used in places where safety standards are strict and non‑negotiable.
Autoclaves are commonly found in:
- Hospitals and clinics
- Diagnostic and pathology laboratories
- Microbiology research labs
- Pharmaceutical manufacturing units
- Educational and research institutions
How an Autoclave Works (Principle)
The working principle of an autoclave is based on moist heat sterilization.
Inside a sealed chamber, water is heated to produce saturated steam. As pressure builds, the steam penetrates instruments, media, and materials placed inside. This heat causes microbial proteins to break down. Once that happens, microorganisms cannot survive.
Steam works better than dry heat because it spreads faster and reaches deeper layers. Anyone who has handled wrapped instruments or culture media knows dry heat alone is not reliable.
This is why autoclaving remains the gold standard.
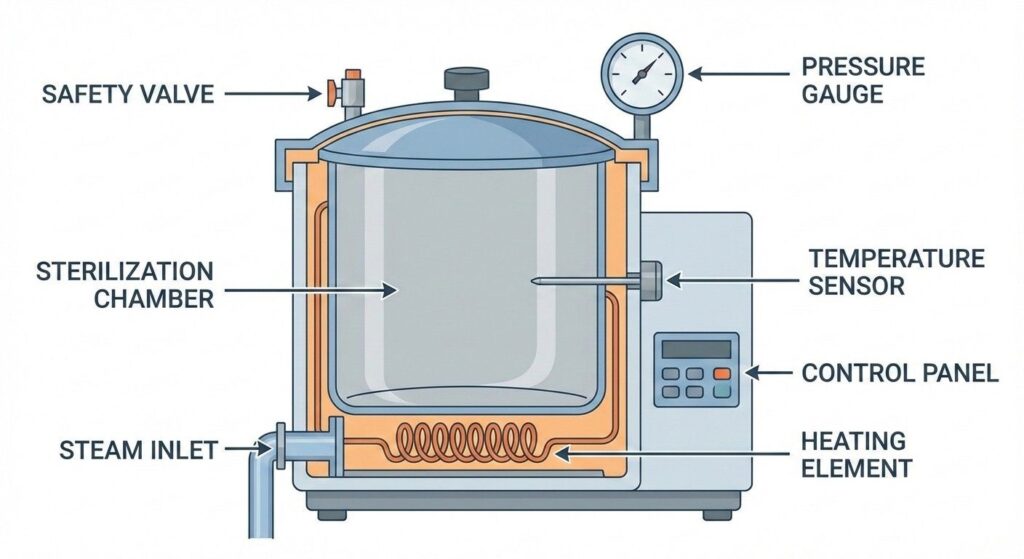
Autoclave Diagram and Main Parts
Understanding the autoclave diagram helps in safe handling and routine checks.
Most autoclaves consist of:
- A heavy-duty sterilization chamber
- Steam or heating system
- Pressure and temperature gauges
- Safety valve
- Control panel for cycle selection
Each part plays a role. If one component fails, sterilization quality drops — which is why maintenance is important.
Autoclave Temperature, Pressure, and Time
Sterilization depends on the correct balance of temperature, pressure, and exposure time.
The most widely used standard cycle is:
- 121°C temperature
- 15 psi pressure
- 15–30 minutes duration
For dense or high‑risk loads, higher settings are applied:
- 132°C temperature
- Around 27 psi pressure
- Shorter cycle times
Running an autoclave below recommended settings can give a false sense of safety. In medical and laboratory environments, that margin for error does not exist.
Types of Autoclave Machines
Autoclaves are designed in different formats depending on usage.
Commonly used types include:
- Gravity displacement autoclaves – used for basic instruments
- Pre‑vacuum autoclaves – suitable for wrapped or porous items
- Vertical autoclaves – compact units for small labs
- Horizontal autoclaves – large-capacity machines for hospitals and pharma plants
Choosing the right type depends on workload, space, and material type.
Uses of Autoclave in Daily Practice
Autoclaves are used wherever contamination control is essential.
In hospitals, they sterilize surgical instruments, dressing trays, and reusable tools.
In laboratories, they are used for glassware, culture media, and decontamination of biological waste.
In pharmaceutical facilities, autoclaves support quality control by sterilizing equipment and materials before production or testing.
Autoclaving in Microbiology
In microbiology, autoclaving is not optional. It is mandatory.
Culture media must be sterile before use. Waste must be neutralized before disposal. Instruments must not carry residues from previous experiments.
Autoclaving helps ensure:
- Reliable culture growth
- Accurate results
- Safe waste handling
- Protection for lab staff
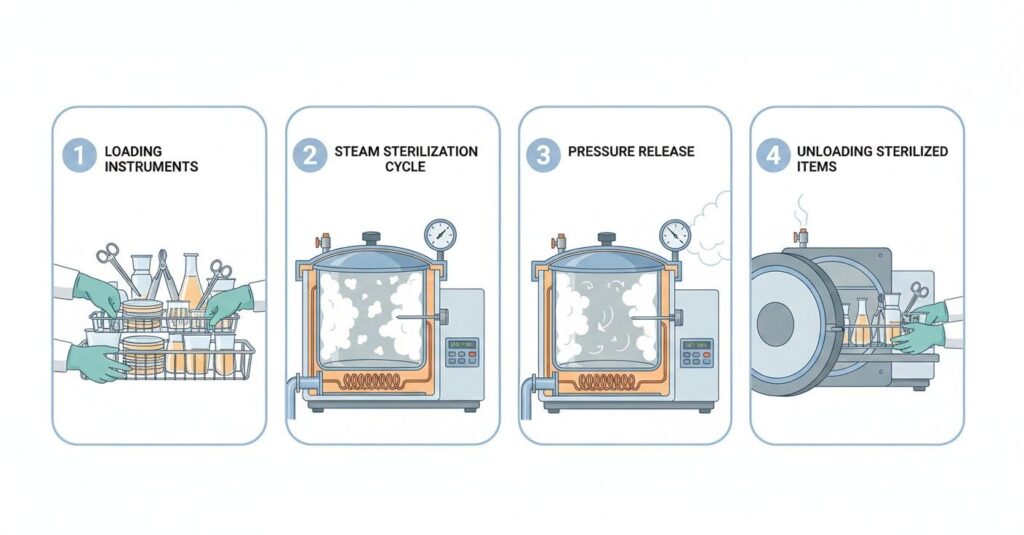
Autoclave Sterilization Process (Step-by-Step)
A typical sterilization cycle follows a fixed sequence.
First, items are cleaned to remove visible debris.
They are then placed in the chamber with enough space for steam flow.
Correct temperature, pressure, and time are selected.
During the cycle, steam penetrates and destroys microorganisms.
After completion, pressure is released gradually.
Only after cooling are items removed.
Skipping steps may save time, but it compromises safety.
Advantages of Autoclave Sterilization
- Consistent and dependable results
- Effective against resistant spores
- No chemical residue
- Environment-friendly method
- Accepted worldwide in medical practice
Autoclave Safety Precautions
- Never overload the chamber
- Always monitor pressure and temperature
- Use heat-resistant gloves
- Do not open the door under pressure
- Schedule regular servicing
These precautions are simple but critical.
Final Thoughts
An autoclave is more than just equipment. It is a safeguard that protects patients, laboratory professionals, and research outcomes.
When used correctly and maintained well, an autoclave quietly performs one of the most important tasks in healthcare and science — keeping environments safe and contamination-free.
Disclaimer:
This content is for informational purposes only. Always follow manufacturer guidelines and professional standards when using or operating autoclave equipment.